Je cadeautjes zeker op tijd in huis hebben voor de feestdagen? Kom langs in onze winkels en vind het perfecte geschenk!
- Afhalen na 1 uur in een winkel met voorraad
- Gratis thuislevering in België vanaf € 30
- Ruim aanbod met 7 miljoen producten
Je cadeautjes zeker op tijd in huis hebben voor de feestdagen? Kom langs in onze winkels en vind het perfecte geschenk!
- Afhalen na 1 uur in een winkel met voorraad
- Gratis thuislevering in België vanaf € 30
- Ruim aanbod met 7 miljoen producten
Zoeken
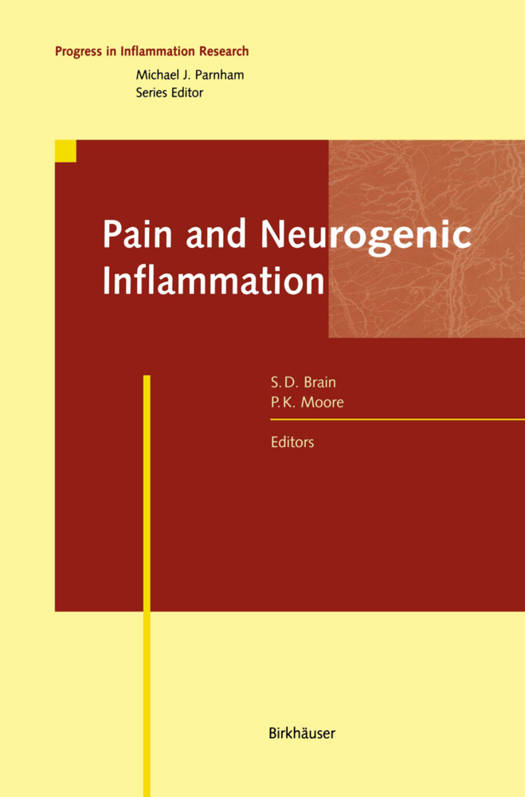
Pain and Neurogenic Inflammation
€ 279,45
+ 558 punten
Omschrijving
Pain and inflammation are inextricably linked phenomena. The observation that chemical mediators with combined pro-inflammatory, algesic and/or hyperalgesic activity occur at the site of inflammation is fundamental not only to our present understanding of the inflammatory process but also to our attempts to devise clini- cally useful anti-inflammatory therapies. Over a hundred years ago it was recognised that primary sensory neurones play a crucially important "dual" role in inflammation. By affecting the transfer of infor- mation from peripheral nociceptors to the spinal cord, a subpopulation of sensory nerves {"pain fibres"} initiate algesia and hyperalgesia, whose sensations are then modified and fine-tuned in the central nervous system. Equally important is the release from the peripheral terminals of sensory neurones of neuropeptides, the acute effects of which are observed as changes in microvascular tone and perme- ability leading to neurogenic inflammation. Over the last decade it has become increasingly clear that this view of the func- tion of sensory nerves is somewhat over-simplified. For example, the mechanisms underlying hyperalgesia may, in certain circumstances, be mimicked in other condi- tions such as the hypersensivity associated with asthma. Furthermore, it has become increasingly evident that over a longer time period the release of neuropeptides from peripheral sensory nerve endings may also have modulating effects on inmune cells and that this may be relevant to chronic inflammatory disease and possibly also to inflammatory hyperalgesia.
Specificaties
Betrokkenen
- Uitgeverij:
Inhoud
- Aantal bladzijden:
- 348
- Taal:
- Engels
- Reeks:
Eigenschappen
- Productcode (EAN):
- 9783034897587
- Verschijningsdatum:
- 10/10/2012
- Uitvoering:
- Paperback
- Formaat:
- Trade paperback (VS)
- Afmetingen:
- 156 mm x 234 mm
- Gewicht:
- 508 g

Alleen bij Standaard Boekhandel
+ 558 punten op je klantenkaart van Standaard Boekhandel
Beoordelingen
We publiceren alleen reviews die voldoen aan de voorwaarden voor reviews. Bekijk onze voorwaarden voor reviews.